Clinical Operational Solutions
Clinical Operational Solutions streamline the research lifecycle through a data-driven, systematic approach. This integrated framework ensures that trials are scientifically sound, logistically viable, and strictly compliant with global regulatory standards. It bridges the gap between a theoretical protocol and a successful, audit-ready trial, ensuring that the Principal Investigator (PI) retains full oversight while delegating technical execution.
Feasibility Assessment
Feasibility is the medical "stress test" of a protocol against real-world clinical practice.
Medical Logic Review: Evaluating if the inclusion/exclusion criteria align with current standard-of-care or if they will create an "un-enrollable" patient population.
Site Infrastructure & Burden: Assessing if your facility has the specialized diagnostics (e.g., specific MRI sequences, cold-chain storage, or infusion suites) and the medical staff bandwidth to execute the study without compromising routine patient care.
Patient Journey Mapping: Visualizing the patient experience to identify potential "drop-out" points, such as overly frequent visits or invasive procedures.
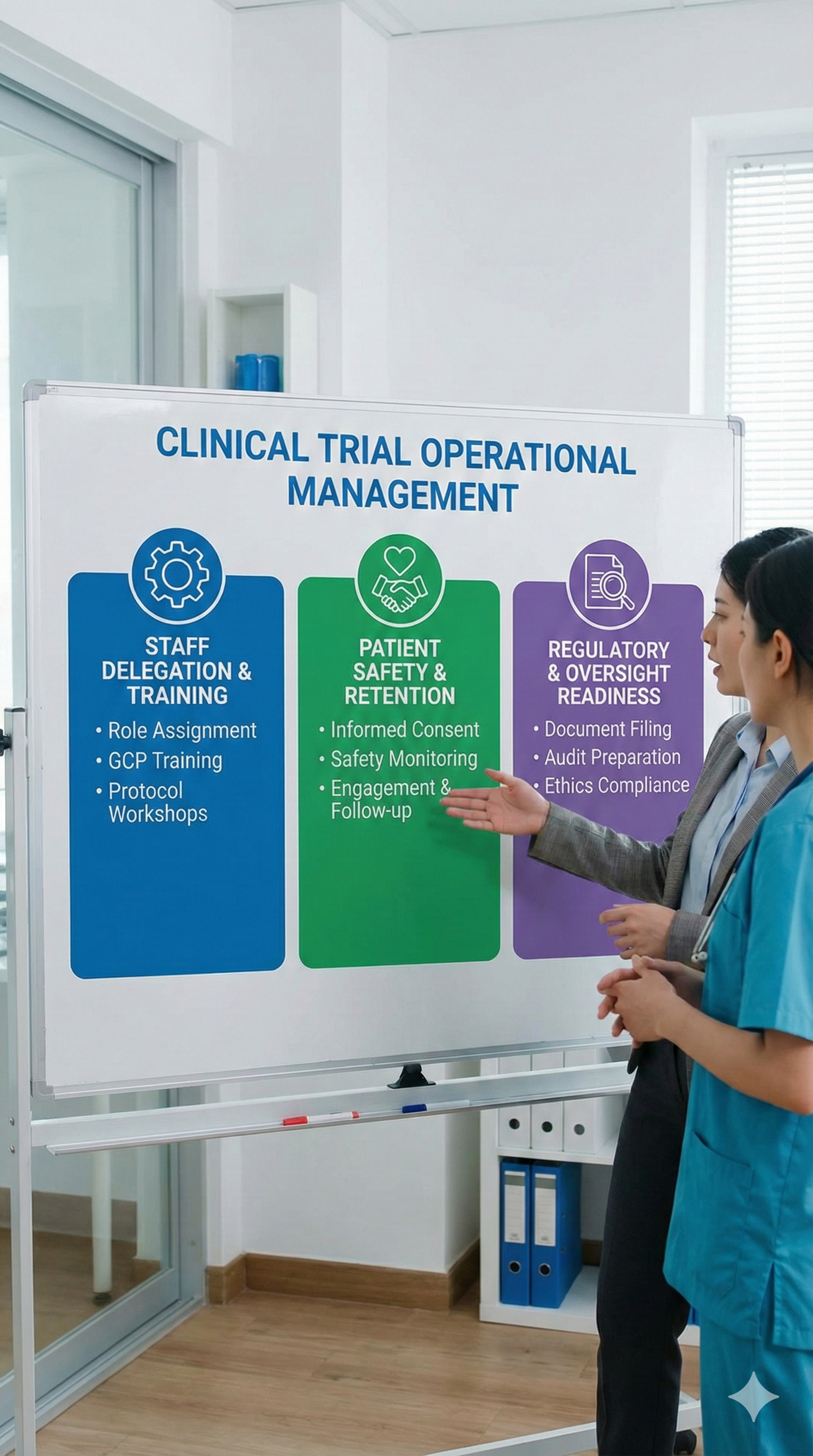
Clinical Trials Operational Management
This is the daily execution of the protocol, where operational efficiency meets clinical excellence.
Staff Delegation & Training: Managing the "Delegation of Authority" (DOA) log to ensure only qualified medical personnel perform specialized tasks (e.g., physical exams, adverse event causality assessments).
Patient Safety & Retention: Implementing digital tools and coordinator support to ensure strict adherence to visit windows, preventing protocol deviations that could jeopardize subject safety or data integrity.
Regulatory & Oversight Readiness: Maintaining a "constant state of audit readiness" through real-time documentation in the Trial Master File (TMF), ensuring that every medical decision made is traceable and justified.
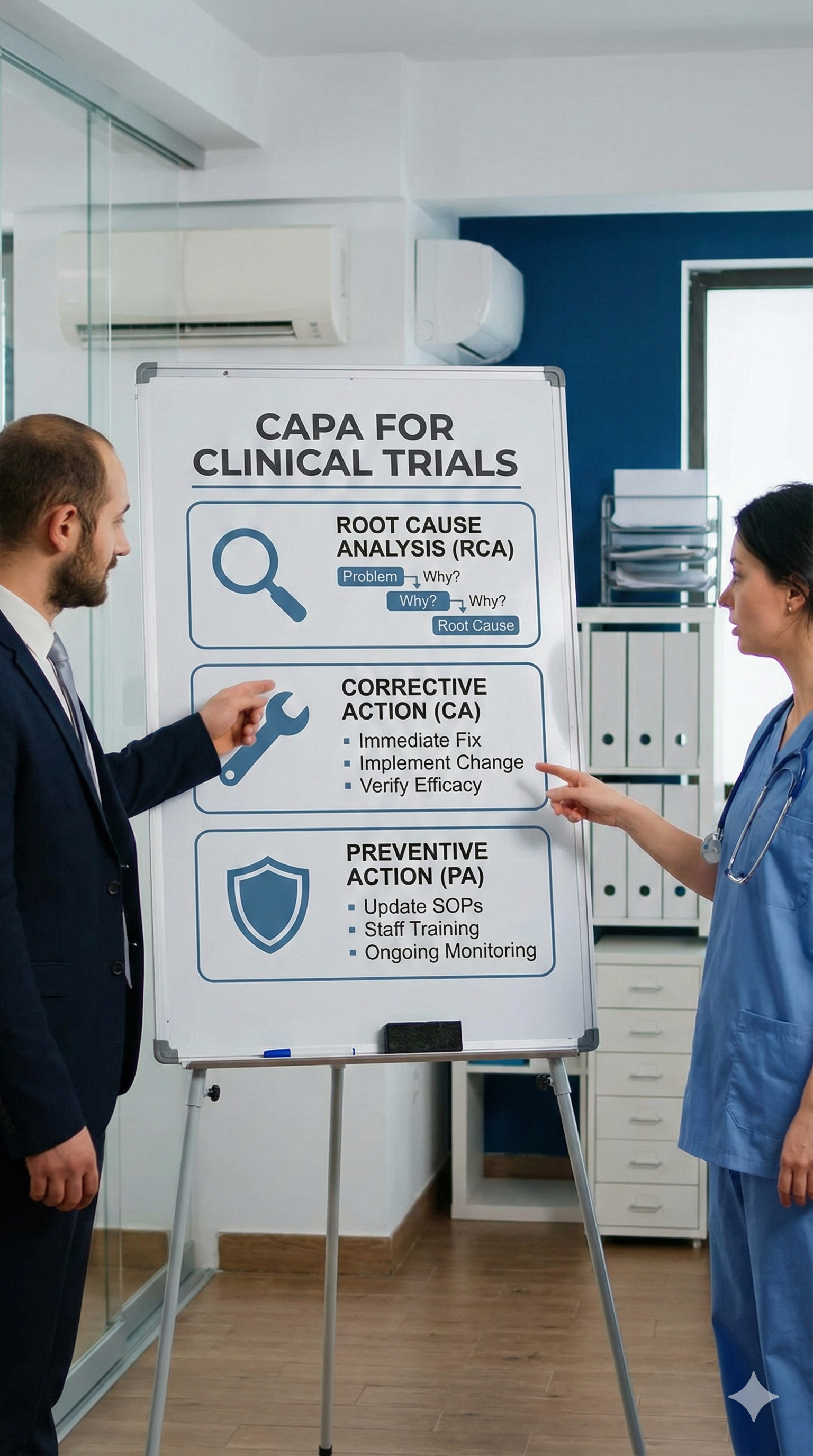
CAPA for Clinical Trials
In the eyes of a doctor, CAPA is the "Morbidity and Mortality (M&M) Report" of clinical research—it is the systematic response to any deviation from the protocol or GCP (Good Clinical Practice).
Root Cause Analysis (RCA): Moving beyond the symptom of an error (e.g., "missing lab sample") to identify the system failure (e.g., "inadequate courier training").
Corrective Action (CA): The immediate medical and administrative fix to resolve the current issue and protect the patient.
Preventive Action (PA): Implementing systemic changes—such as updated SOPs, new staff training, or automated alerts—to ensure the same error never recurs across the site.